
Patients with scores ≤30 were likely to have structural disorders alone, whereas those with scores >60 were likely to have functional or psychiatric disorders, with or without coexisting structural conditions.", Conclusions: In this tertiary cohort, categories of illnesses had large effects on total DHI scores. DHI≤30 (mild handicap) had specificity=0.98 for structural disorders alone, whereas DHI>60 (severe handicap) had specificity=0.88 for functional or psychiatric disorders. Results: Mean DHI scores differed significantly by diagnostic category (structural 35☑8, functional 64☑5, and psychiatric 65☑9), before and after adjusting for age and sex ( p1.62 for structural versus functional and psychiatric categories). Sensitivities and specificities of DHI scores for identifying structural versus functional or psychiatric disorders were calculated.

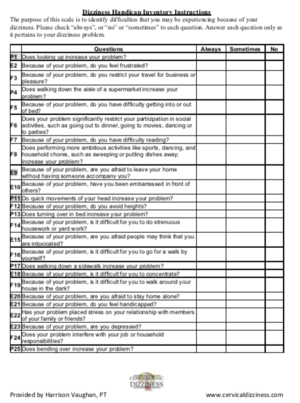
DHI scores were compared across diagnostic categories. Main Outcome Measure(s): Active illnesses identified by a multidisciplinary neurotology team were abstracted from medical records, cataloged as structural, functional, or psychiatric disorders, and used to group patients into diagnostic categories: structural (structural disorders only), functional (functional disorders with/without structural disorders), and psychiatric (psychiatric disorders with/without other conditions). Patients: Eighty-five patients who underwent multidisciplinary neurotologic evaluations. This study investigated the relationship between total DHI scores and the presence of structural, functional, and psychiatric disorders in tertiary neurotology patients. DHI scores do not correlate with severity of structural vestibular deficits thus, high DHI scores may reflect other causes of morbidity. Patients with scores ≤30 were likely to have structural disorders alone, whereas those with scores >60 were likely to have functional or psychiatric disorders, with or without coexisting structural conditions.Ībstract = "Objective: The Dizziness Handicap Inventory (DHI) is a 25- item self-report quantifying dizziness-related physical and emotional symptoms and restrictions in daily activities.

( Arch Otolaryngol Head Neck Surg.Objective: The Dizziness Handicap Inventory (DHI) is a 25- item self-report quantifying dizziness-related physical and emotional symptoms and restrictions in daily activities. With the exception of the physical subscale, the mean values for DHI scale scores increased significantly with increases in the frequency of dizziness episodes. The final version of the DHI was administered to 106 consecutive patients and demonstrated good internal consistency reliability. Cronbach's α coefficient was employed to measure reliability based on consistency of the preliminary version. The items were subgrouped into three content domains representing functional, emotional, and physical aspects of dizziness and unsteadiness. The development of the preliminary (37 items) and final versions (25 items) of the DHI are described. The 25-item Dizziness Handicap Inventory (DHI) was developed to evaluate the selfperceived handicapping effects imposed by vestibular system disease.


 0 kommentar(er)
0 kommentar(er)
